Part of Carebook’s Global Blog Series: The Future of Pharmacy
Andrew Matthews, a Director at the Australian Digital Health Agency, shares how Australia’s future-facing digital health strategy accelerated with the global COVID-19 crisis—and is succeeding with a people-centric approach.
“Co-design involves working together to design a new product [or process], making full use of each other’s knowledge, resources and contributions, to achieve better outcomes or improved efficiency.”— NCBI Using Co-Design to Develop a Collective Leadership Intervention for Healthcare Teams to Improve Safety Culture (1)(2)
ACCELERATING INNOVATION
“Instead of months, we had just 8 weeks to make this happen.”
Even before the COVID-19 crisis hit in March 2020, Australia’s Digital Health Agency was working hard to advance its innovation strategy in the realm of digital health. Australia’s centralized, connected “My Health Record” program was gaining momentum—its people-centric mandate to help every Australian and their family consolidate health information into one easy-to-access place. And along with this initiative, progress was being made in the country’s move towards laying the foundation for Telehealth and Electronic prescriptions. This trifecta of future-forward plans was in motion, actively addressing the need to make healthcare even more accessible to everyone in Australia.
With the goal to tackle some large, fundamental health system challenges—for individuals, pharmacists, and physicians alike—for several years prior to the pandemic, electronic prescriptions (or ePrescriptions) were on the roadmap as part of a broad digital health and medicines safety framework in Australia, a country with subsidized healthcare. ePrescriptions enable the prescribing, dispensing and claiming of medicines, without the need for a paper prescription—allowing a fully digital version of a prescription to be sent directly to a person’s mobile phone (or email) for dispensing at their pharmacy of choice. Benefits of ePrescriptions include easier accessibility, time savings, and increased medicine safety.
Andrew Matthews says that between 2018–2020, their team had developed a robust technical framework, which included the solution architecture, conformance assessment scheme and conformance profile under a co-design process, to start piloting an ePrescription program as a critical part of the tele-health initiative. “Prior to 2020, the preliminary tech framework was done and it meant that regulatory changes (nationally and for each state/territory) were next on the list. Round table talks were still in progress.” Matthews said that, specifically, the bushfires in 2019 had once again spotlighted the challenge of people and medical professionals living in remote places. “To round out the tele-health experience, paper-free options for prescriptions were slated for rollout in 2022. But when the COVID-19 plan came about in early 2020, the ePrescriptions program was fast-tracked. Instead of months, we had just 8 weeks to make this happen.”
SUCCESS WITH A CO-DESIGN APPROACH
“People always want to know how things will impact them.”
At the best of times, a co-design approach to healthcare can be challenging. Through the meaningful involvement of users (primary and peripheral), it draws upon design thinking to bring people together to improve quality of care.
Implementation of co-design within the healthcare realm aims to cut out “waste” produced when research and development doesn’t properly consider the real people who will use a system.
Matthews notes that he considers their co-design approach as one of the reasons their digital health strategy found success. “From the start, we considered and supported physicians, pharmacists, patients and their families with the changes we rolled out. Change is hard. People always want to know how things will impact them. And because we made people the core consideration of these new initiatives, we were able to implement our plans very quickly—some said 5 years of digitalization moved forward in a few months.”
FROM MICRO-COMMUNITIES TO WHOLE-COUNTRY ADOPTION
“Pharmacists tend to be strong adopters of digital initiatives.”
As new demands for tele-health options grew with the spread of COVID, and with the initial technical foundation done, Australia’s Digital Health Agency found that the previous barriers in the way of implementing ePrescriptions melted away. “People who were hesitant before the crisis became the cheerleaders for this digital innovation. It was clear that greater accessibility meant better care for everyone.”
Matthews says their first priority for adoption of ePrescriptions was making pharmacies ready. Pharmacists, after all, are a pivotal point of accessible care, a critical link between doctors and patients. “One of the best things about the pharmacy sector is that pharmacists tend to be strong adopters of digital initiatives. Plus, from a functional standpoint, our national requirements stated that every person must be able to fill their prescriptions at the pharmacy of their choice.” To test the user experiences, the Digital Health Agency set up “micro-communities”. Their goal was to see and fix flaws, get feedback, and build confidence in the program.
“We knew a “top down” approach wouldn’t be ideal,” says Matthews. “We didn’t want the government to tell people that the new system worked. Instead, we put the program into the hands of real communities and allowed them to use it and provide real feedback. In the end, it was the people—from patients to pharmacists to doctors—who were nodding their heads and telling others that it worked. And while that was happening and confidence was growing within these smaller test communities, a second-wave COVID-19 outbreak hit Victoria. This is where we supported the general release of software across Victoria to serve people who were isolating. That really started the widespread adoption.”
COMMUNICATION IS KING
“Empowerment is the foundation of success.”
Michael Charlton, part of the media team for the Agency’s Medicines Safety Program, says the co-design approach didn’t end with the implementation of the new technology. “It was critical that everyone needed to understand the functionality—and feel comfortable using it. We worked hard to hear feedback and empower people using real language for training documents.” Matthews notes that they employed a wide range of practising health professionals to curate the everyday language around the program. “Empowerment is the foundation of success. General practitioners, pharmacists, consumers—a diverse cross-section of people—were consulted about the best way to enable all the users of this system with the information they needed to be fully informed.”
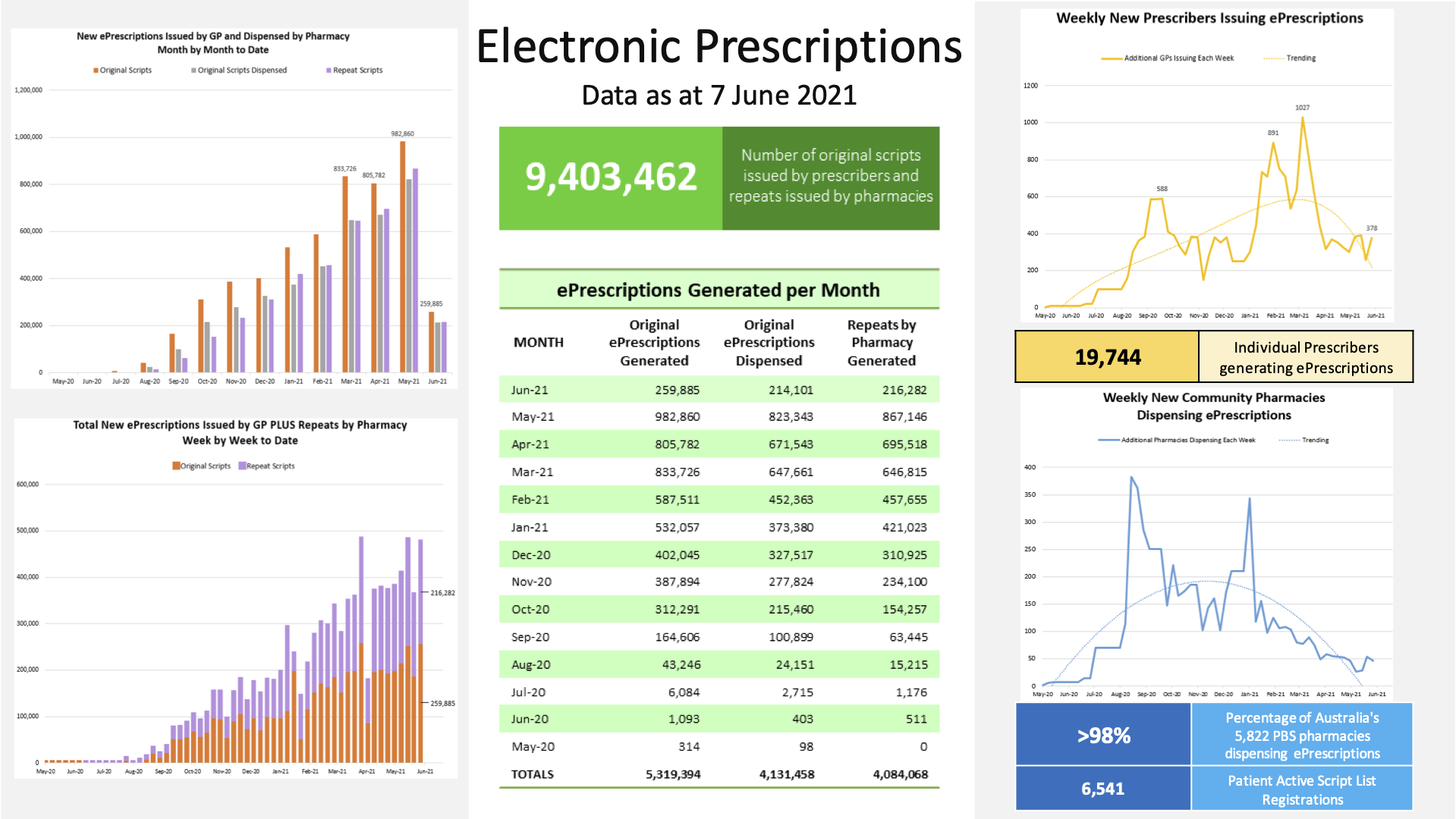
Growth Data
FUTURE-FORWARD: THE DIGITAL INNOVATION CONTINUES
Smooth implementation of ePrescriptions is an important part of Australia’s digital health strategy for many reasons: it improves remote access; strengthens the tele-health experience; and, as part of the medicines safety strategy, aims to reduce errors and adverse events with medication. In fact, in 2017, Australia became part of the WHO-led push to cut medication errors in half by 2020.
“In Australia, approximately 250,000 hospital admissions per annum come as a result of medication-related incidents.”(3) When pharmacists are not involved, studies show medication errors are more likely. Pharmacists, who have the ability to review medications and proactively intervene, play a big part in reducing medication errors and improving patient care and health outcomes.
Improved medication adherence is yet another box that the adoption of ePrescriptions ticks. In fact, pharmacist-led initiatives in Australia have had astounding results, according to a 2019 study documented in the National Institute of Health. “The total national cost of medication non-adherence across three prevalent conditions, hypertension, dyslipidemia and depression was $10.4 billion equating to $517 per adult. Following enrollment in the pharmacist-led intervention medication non-adherence costs per adult decreased $95 saving the Australian health care system and patients $1.9 billion annually.”(4)
THE FUTURE OF CARE IN AUSTRALIA
While the digital health strategy is leading the way in terms of a cohesive foundation and successful rollout, Matthews notes that their current digital health strategy continues to expand its reach with increasing adoption rates. With core objectives such as safety and accessibility, Australia’s Digital Health Agency will optimize their current programs and continue to move forward. Matthews says implementation across the aged cared and hospital sectors (beyond primary care) are where they will focus ePrescriptions next.
About Andrew Matthews

Andrew Matthews is a Director at the Australian Digital Health Agency and is responsible for the Agency’s delivery of the Medicines Safety strategic priority in the National Digital Health Strategy’s ‘Framework for Action’. Electronic prescribing and the implementation of ePrescriptions is a priority action under this strategy.
Andrew has been both a hospital and community pharmacist and worked in Adelaide, Canberra, and Wagga Wagga. His previous employment has included successful delivery of health & pharmacy programs and projects across organisations such as the Pharmacy Guild of Australia, the Society of Hospital Pharmacists of Australia and the Australian Pharmacy Council.
Australian Digital Health Agency Web: www.digitalhealth.gov.au
Email: help@digitalhealth.gov.au
Agency help line: 1300 901 001
LinkedIn: linkedin.com/company/australian-digital-health-agency Facebook: https://www.facebook.com/AuDigitalHealth
Twitter: twitter.com/AuDigitalHealth
About Carebook
Today, Carebook offers a proven digital health platform with powerful features including medication management, health and wellness, retail and loyalty, and more. Pull together your revenue streams into one, single spot—your customer’s hands. And Carebook is already planning for tomorrow with medication AI research with two important Canadian Universities and new, integrated rPPG technology that measures vital signs using only a smartphone. To find out how Carebook can help your organization lead digital health and wellness today and tomorrow, please contact Howard Fried.
Web: www.carebook.com
LinkedIn: https://www.linkedin.com/company/carebook-technologies-inc-
Facebook French): https://www.facebook.com/CarebookTechnologiesFR
Facebook English): https://www.facebook.com/CarebookTechnologies
Twitter: https://twitter.com/CarebookT @carebookT
Medium: https://carebook.medium.com/
(1)Bovaird T., Loeffler E. From engagement to co-production: How users and communities contribute to public services. In: Brandsen T., Pestoff V., editors. New Public Governance, the Third Sector and Co-Production. Routledge; London, UK: 2012.
(3) Kyle Malone, Pharmacist, MPharms MPSI, Medication Safety in Australia and the Learning Health System Approach looks at how medication safety in Australia can be improved by implementing a learning health system. https://www.pharmapodhq.com/resources/medication-safety-in-australia-and- the-learning-health-system-approach/
(4)Cutler R.L., Torres-Robles A., Wiecek E., Drake B., et.al. Pharmacist-led medication non-adherence intervention: reducing the economic burden placed on the Australian health care system. Patient Prefer Adherence. 2019; 13; 853-862.

